
Irritable bowel syndrome (IBS) affects millions of people around the world, causing significant discomfort and routine disruptions in daily life. It’s predominantly characterized by abdominal pain, as well as altered bowel habits.
If you’re one of the millions of Americans who deal with IBS, you’ve likely wondered how long the condition lasts and what you can do to reduce some of its worst symptoms.
Although there is no permanent cure for IBS, there are certain steps you can take to prevent and shorten flare-ups. Let’s discuss the factors that influence this syndrome and what you can do about them.
Understanding IBS: Causes & Triggers
Some mistake irritable bowel syndrome for gastroparesis or GERD, but these are all different conditions.
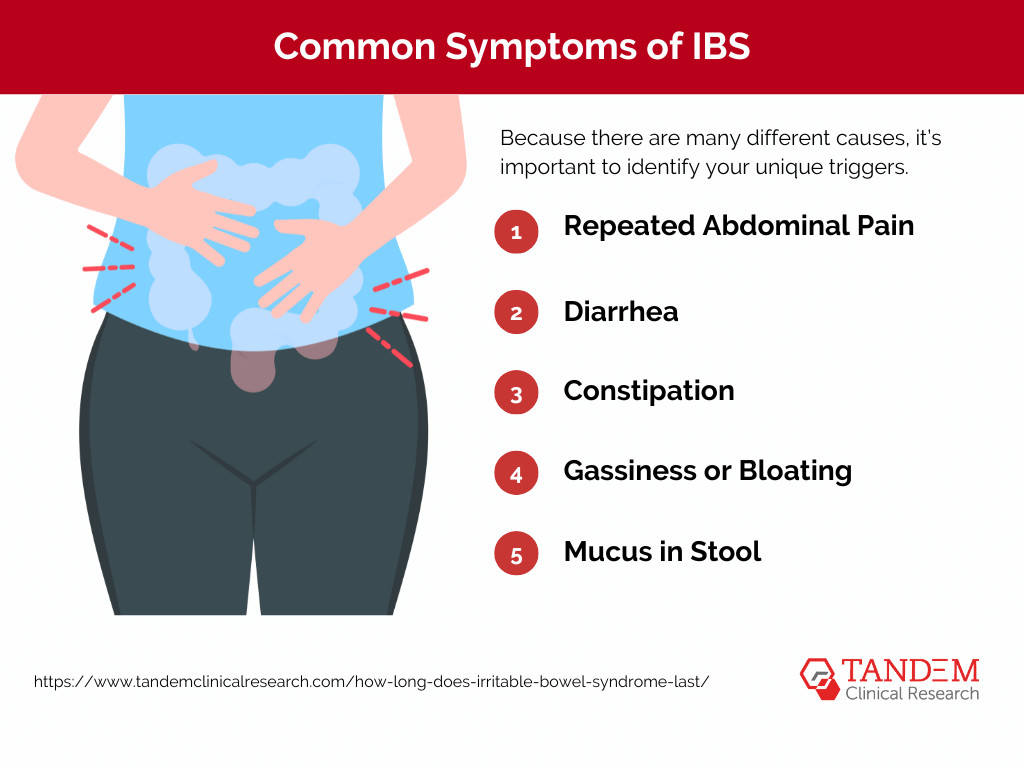
IBS is a group of symptoms that occur together, including repeated pain in your abdomen and changes in your bowel movements, which may be diarrhea, constipation, or both. Many patients experience these symptoms without any visible signs of damage or disease.
While the exact cause of IBS isn’t entirely understood, various factors can contribute to its development, including:
- Gut motility issues
- Visceral hypersensitivity
- Imbalances in gut microbiota
Because there are many different causes, it’s important to identify your unique triggers. Doing so will help effectively target and minimize your symptoms over the course of your lifetime.
IBS triggers also vary among individuals but commonly include dietary factors (such as certain foods or beverages), stress, hormonal changes, and gut infections. Recognizing these concerns empowers you to make informed lifestyle choices and adjustments to alleviate symptoms and, in some cases, shorten the duration of IBS flare-ups.
Subtypes of IBS and Its Symptoms
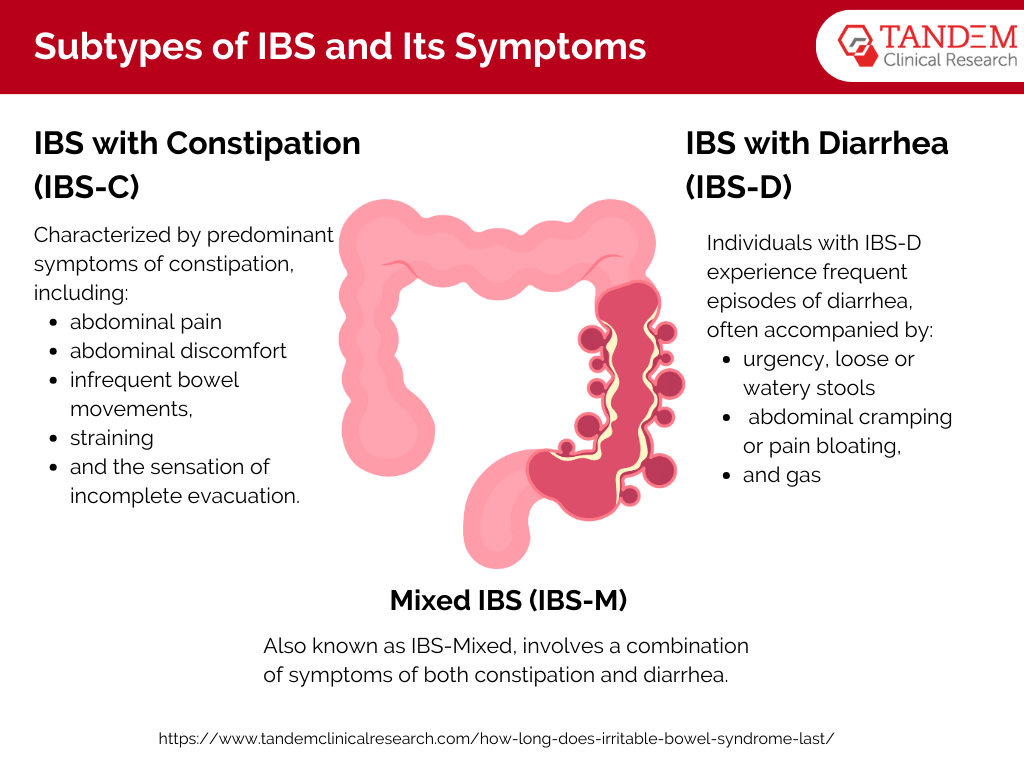
There are several recognized types of IBS, each with distinct symptom profiles:
IBS with Constipation (IBS-C): This subtype of IBS is characterized by predominant symptoms of constipation, including infrequent bowel movements, straining during bowel movements, and the sensation of incomplete evacuation. Patients with IBS-C may also experience abdominal discomfort or pain, bloating, and gas.
IBS with Diarrhea (IBS-D): Individuals with IBS-D experience frequent episodes of diarrhea, often accompanied by urgency, loose or watery stools, and abdominal cramping or pain. Bloating and gas may also be present in some cases.
Mixed IBS (IBS-M): Mixed IBS, also known as IBS-Mixed, involves a combination of symptoms of both constipation and diarrhea. Patients with IBS-M may alternate between episodes of constipation and diarrhea, with varying degrees of severity and frequency.
Factors Influencing the Duration of IBS
The duration of IBS varies greatly among individuals, influenced by factors such as the severity of symptoms, response to treatment, and overall health status.
While some individuals may experience intermittent symptoms that resolve with lifestyle modifications and dietary changes, others may face persistent challenges requiring ongoing medical management.
Treatment approaches for IBS encompass a spectrum of interventions, including dietary modifications), medications, and complementary therapies.
Tips for Managing and Coping with IBS
Managing IBS typically involves a multifaceted approach. Let’s explore the different treatment strategies and how they can impact the duration and frequency of IBS flare-ups.
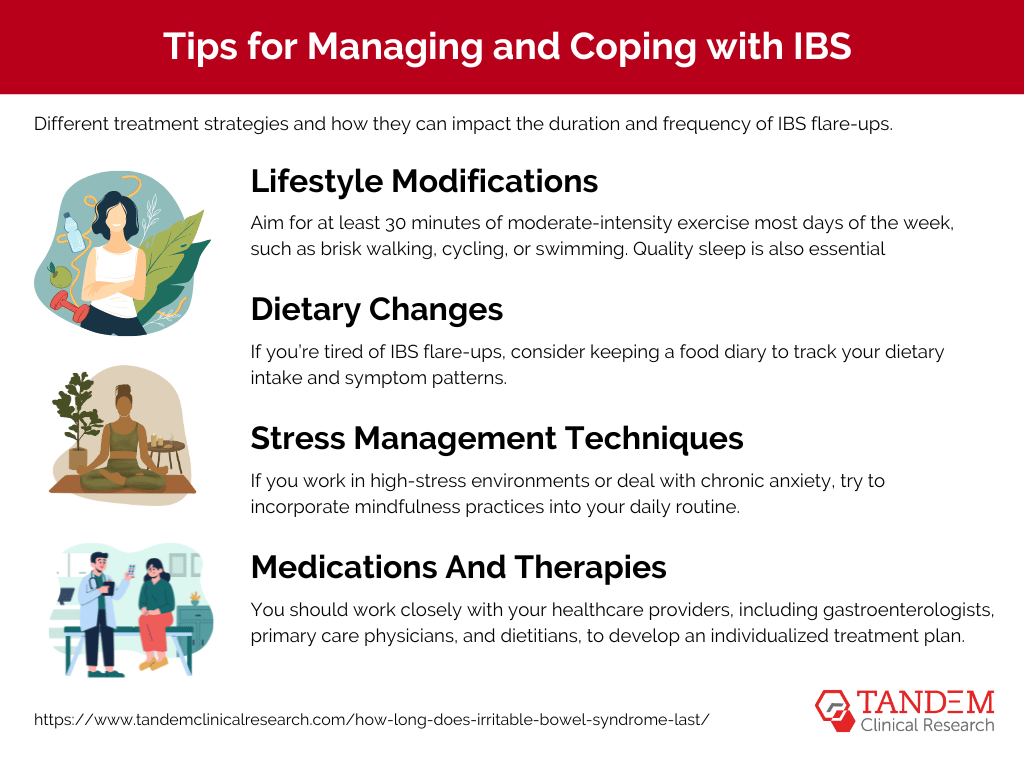
Lifestyle Modifications
Engaging in regular physical activity can help regulate bowel function, reduce stress levels, and improve overall digestive health. Aim for at least 30 minutes of moderate-intensity exercise most days of the week, such as brisk walking, cycling, or swimming.
Quality sleep is also essential for managing IBS symptoms and promoting overall health. Establish a consistent sleep schedule, create a relaxing bedtime routine, and ensure your sleep environment is conducive to great rest.
Dietary Changes
If you’re tired of IBS flare-ups, consider keeping a food diary to track your dietary intake and symptom patterns. This will help you trigger foods that exacerbate your symptoms, such as high-fat foods, spicy foods, caffeine, alcohol, and artificial sweeteners.
Some IBS patients also follow a low-FODMAP diet under the guidance of a registered dietitian. This involves temporarily restricting fermentable carbohydrates that can contribute to IBS symptoms and gradually reintroducing them to identify specific triggers.
Regardless of your dietary approaches, be sure to drink plenty of water throughout the day. It’s also a good idea to limit your intake of carbonated beverages and caffeine, which can both exacerbate bloating and discomfort.
Stress Management Techniques
Although stress does not cause IBS, it can exacerbate flare-ups.
If you work in high-stress environments or deal with chronic anxiety, try to incorporate mindfulness practices into your daily routine. These include deep breathing exercises, progressive muscle relaxation, or guided imagery.
You may also want to consider stress-reduction techniques such as yoga, meditation, tai chi, or aromatherapy. These activities can help calm the mind, reduce muscle tension, and alleviate stress-related gastrointestinal symptoms.
In fact, a recent 2023 study found that regular yoga practice specifically improved IBS symptoms in participants. Although practicing in an in-person studio might be best, the study found that virtual yoga can also potentially increase effective management therapies for IBS patients.
IBS can feel frustrating and disheartening, but remember that you have friends and family members in your corner. If you start to feel down, reach out to your loved ones or consider joining support groups for emotional support and understanding. Sharing experiences with others can help you find validation, encouragement, and practical coping strategies.
Medications And Therapies
Lastly, you should work closely with your healthcare providers, including gastroenterologists, primary care physicians, and dietitians, to develop an individualized treatment plan.
Discuss the potential benefits and risks of medications commonly used to manage IBS symptoms, such as antispasmodics, laxatives, antidiarrheals, and antidepressants. Your healthcare provider can help determine the most appropriate medication regimen for you.
You may also want to explore complementary therapies such as probiotics, acupuncture, hypnotherapy, or cognitive-behavioral therapy (CBT). These can address underlying psychological factors and promote additional symptom relief.
Help Researchers Study & Develop IBS Treatments
IBS currently lasts for life, but that might not always be the case.
If you want to help doctors learn more about IBS and its potential causes, triggers, and treatments, consider joining a clinical trial.
Clinical trials play a vital role in evaluating the safety and efficacy of all kinds of therapies, paving the way for new treatment options for individuals with IBS, and changing how we view the condition.
Legitimate clinical trials adhere to strict ethical and regulatory standards to safeguard participants’ well-being and ensure the integrity of the research findings. By participating in one, you won’t just contribute to great research – you’ll also gain access to cutting-edge treatments that could positively impact your own symptoms.
Get Matched With Tandem Clinical Research Today
Navigating life with IBS can be challenging, to say the least. Still, understanding the condition and its triggers can help you manage flare-ups as much as possible.
If you’re interested in joining a clinical study for irritable bowel syndrome, let’s connect. Tandem Clinical Research helps individuals get involved with various research opportunities, including clinical trials of the most innovative IBS treatments.







